-
Table of Contents
- What Should I Do If Azithromycin Doesn’t Work?
- Understanding Azithromycin Resistance
- Signs That Azithromycin Is Not Working
- Steps to Take If Azithromycin Is Ineffective
- 1. Consult Your Healthcare Provider
- 2. Get a Culture Test
- 3. Explore Alternative Antibiotics
- 4. Consider Adjunctive Therapies
- Case Studies and Statistics
- Conclusion
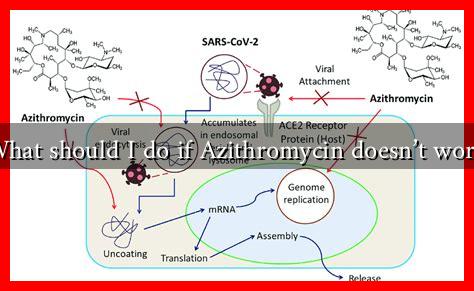
What Should I Do If Azithromycin Doesn’t Work?
Azithromycin is a widely used antibiotic that belongs to the macrolide class. It is commonly prescribed for various bacterial infections, including respiratory infections, skin infections, and sexually transmitted diseases. However, there are instances when azithromycin may not be effective. This article explores the steps you should take if you find that azithromycin is not working for your condition.
Understanding Azithromycin Resistance
Before diving into what to do if azithromycin fails, it’s essential to understand why this might happen. Antibiotic resistance is a growing concern in the medical community. Bacteria can develop resistance to antibiotics through various mechanisms, including:
- Genetic mutations that alter the target site of the antibiotic.
- Enzymatic degradation of the antibiotic.
- Efflux pumps that expel the antibiotic from the bacterial cell.
According to the Centers for Disease Control and Prevention (CDC), antibiotic resistance is responsible for at least 2.8 million infections and 35,000 deaths each year in the United States alone. This highlights the importance of using antibiotics judiciously and understanding when they may not be effective.
Signs That Azithromycin Is Not Working
Recognizing the signs that azithromycin is not effective is crucial for timely intervention. Some indicators include:
- Persistent or worsening symptoms after 48-72 hours of treatment.
- Development of new symptoms that were not present before starting the antibiotic.
- Fever that does not subside or returns after initial improvement.
If you experience any of these symptoms, it may be time to consult your healthcare provider.
Steps to Take If Azithromycin Is Ineffective
If you find that azithromycin is not working for you, consider the following steps:
1. Consult Your Healthcare Provider
Your first course of action should be to contact your healthcare provider. They can assess your symptoms and determine whether a different antibiotic or treatment plan is necessary. It’s essential to provide them with detailed information about your symptoms, medical history, and any other medications you are taking.
2. Get a Culture Test
Your doctor may recommend a culture test to identify the specific bacteria causing your infection. This test can help determine which antibiotics will be most effective. For example, if you have a respiratory infection, a sputum culture can reveal whether the bacteria are resistant to azithromycin.
3. Explore Alternative Antibiotics
If azithromycin is ineffective, your healthcare provider may prescribe an alternative antibiotic. Some common alternatives include:
- Amoxicillin
- Ciprofloxacin
- Doxycycline
Each of these antibiotics works differently and may be more effective against certain types of bacteria.
4. Consider Adjunctive Therapies
In some cases, adjunctive therapies may be beneficial. For instance, if you have a respiratory infection, your doctor might recommend bronchodilators or corticosteroids to help alleviate symptoms while addressing the underlying infection.
Case Studies and Statistics
Research has shown that antibiotic resistance is a significant issue. A study published in the Journal of Antimicrobial Chemotherapy found that azithromycin resistance in Streptococcus pneumoniae has increased from 0% in 1999 to over 30% in some regions by 2018. This underscores the importance of monitoring resistance patterns and adjusting treatment accordingly.
Conclusion
In summary, if azithromycin does not work for your infection, it is crucial to take proactive steps. Consult your healthcare provider, consider getting a culture test, explore alternative antibiotics, and discuss adjunctive therapies. Understanding the reasons behind antibiotic resistance and recognizing the signs of treatment failure can lead to more effective management of bacterial infections. Always remember that antibiotics should be used responsibly to combat the growing threat of resistance.
For more information on antibiotic resistance and its implications, visit the CDC’s Antibiotic Resistance page.