-
Table of Contents
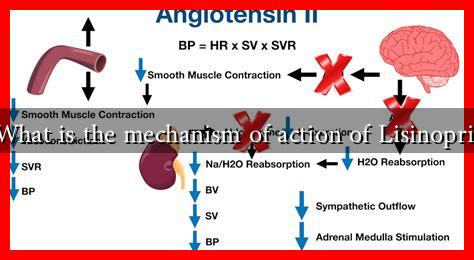
What is the Mechanism of Action of Lisinopril?
Lisinopril is a widely prescribed medication primarily used to treat high blood pressure (hypertension) and heart failure. As an angiotensin-converting enzyme (ACE) inhibitor, it plays a crucial role in the management of cardiovascular diseases. Understanding the mechanism of action of Lisinopril can provide valuable insights into its therapeutic effects and potential side effects.
Understanding the Renin-Angiotensin-Aldosterone System (RAAS)
To grasp how Lisinopril works, it is essential to understand the Renin-Angiotensin-Aldosterone System (RAAS), a hormone system that regulates blood pressure and fluid balance. The key components of RAAS include:
- Renin: An enzyme released by the kidneys in response to low blood pressure or low sodium levels.
- Angiotensin I: A peptide formed when renin converts angiotensinogen (produced by the liver) into angiotensin I.
- Angiotensin II: A potent vasoconstrictor formed when angiotensin I is converted by ACE.
- Aldosterone: A hormone released by the adrenal glands that promotes sodium and water retention, increasing blood volume and pressure.
The Role of Lisinopril in RAAS
Lisinopril inhibits the action of ACE, which is responsible for converting angiotensin I into angiotensin II. By blocking this conversion, Lisinopril effectively reduces the levels of angiotensin II in the bloodstream. This leads to several physiological effects:
- Vasodilation: Lower levels of angiotensin II result in the relaxation of blood vessels, which decreases vascular resistance and lowers blood pressure.
- Reduced Aldosterone Secretion: With less angiotensin II, the adrenal glands secrete less aldosterone, leading to decreased sodium and water retention.
- Decreased Cardiac Workload: By lowering blood pressure and reducing fluid overload, Lisinopril decreases the workload on the heart, making it beneficial for patients with heart failure.
Clinical Applications of Lisinopril
Lisinopril is used in various clinical scenarios, including:
- Hypertension: It is effective in lowering blood pressure, which can reduce the risk of stroke, heart attack, and kidney problems.
- Heart Failure: Lisinopril helps improve symptoms and prolong survival in patients with heart failure by reducing the heart’s workload.
- Post-Myocardial Infarction: It is often prescribed after a heart attack to improve survival rates and prevent further cardiac events.
Case Studies and Statistics
Numerous studies have demonstrated the efficacy of Lisinopril in managing hypertension and heart failure. For instance, a study published in the New England Journal of Medicine found that patients treated with Lisinopril after a heart attack had a significantly lower risk of mortality compared to those who did not receive the medication. Additionally, the American Heart Association reports that ACE inhibitors like Lisinopril can reduce the risk of heart failure hospitalization by up to 30%.
Potential Side Effects and Considerations
While Lisinopril is generally well-tolerated, it can cause side effects in some patients. Common side effects include:
- Dizziness or lightheadedness
- Cough
- Elevated potassium levels (hyperkalemia)
- Angioedema (swelling of deeper layers of the skin)
Patients should be monitored for these side effects, especially those with pre-existing kidney conditions or those taking other medications that affect potassium levels.
Conclusion
Lisinopril is a vital medication in the management of hypertension and heart failure, primarily functioning through its inhibition of the ACE enzyme within the RAAS. By reducing levels of angiotensin II, Lisinopril promotes vasodilation, decreases fluid retention, and ultimately lowers blood pressure. Its clinical applications are supported by robust evidence, demonstrating significant benefits for patients at risk of cardiovascular events. However, like all medications, it is essential to consider potential side effects and monitor patients accordingly. Understanding the mechanism of action of Lisinopril not only enhances patient care but also empowers individuals to engage in informed discussions with their healthcare providers.