-
Table of Contents
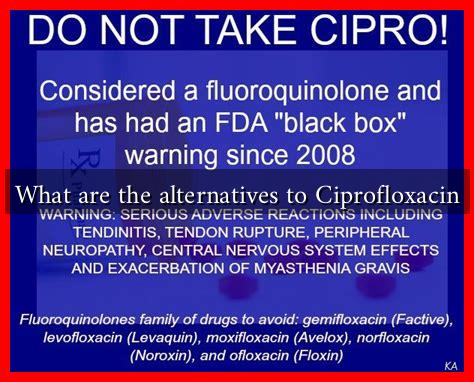
- What are the Alternatives to Ciprofloxacin?
- Understanding Ciprofloxacin
- Alternative Antibiotics
- 1. Nitrofurantoin
- 2. Trimethoprim-Sulfamethoxazole (TMP-SMX)
- 3. Amoxicillin-Clavulanate
- 4. Levofloxacin
- Non-Antibiotic Alternatives
- Case Studies and Statistics
- Considerations for Choosing Alternatives
- Conclusion
What are the Alternatives to Ciprofloxacin?
Ciprofloxacin, a fluoroquinolone antibiotic, has been widely used to treat various bacterial infections, including urinary tract infections, respiratory infections, and skin infections. However, due to rising concerns over antibiotic resistance and potential side effects, healthcare providers are increasingly seeking alternatives. This article explores the alternatives to ciprofloxacin, their effectiveness, and considerations for their use.
Understanding Ciprofloxacin
Ciprofloxacin works by inhibiting bacterial DNA gyrase and topoisomerase IV, enzymes critical for bacterial replication. While effective, its use has been associated with several adverse effects, including:
- Tendon damage
- Neuropathy
- Gastrointestinal disturbances
- Potential for serious allergic reactions
Moreover, the overuse of ciprofloxacin has contributed to the emergence of resistant bacterial strains, making it imperative to explore alternative treatment options.
Alternative Antibiotics
Several antibiotics can serve as alternatives to ciprofloxacin, depending on the type of infection and the susceptibility of the bacteria involved. Here are some notable options:
1. Nitrofurantoin
Nitrofurantoin is primarily used for urinary tract infections (UTIs). It works by damaging bacterial DNA and is particularly effective against E. coli, the most common UTI pathogen. Studies have shown that nitrofurantoin has a lower risk of resistance compared to fluoroquinolones.
2. Trimethoprim-Sulfamethoxazole (TMP-SMX)
This combination antibiotic is effective against a variety of bacterial infections, including UTIs and respiratory infections. TMP-SMX works by inhibiting bacterial folic acid synthesis. However, resistance patterns should be evaluated before prescribing this medication.
3. Amoxicillin-Clavulanate
Amoxicillin-clavulanate is a broad-spectrum antibiotic that can treat infections caused by both gram-positive and gram-negative bacteria. It is often used for respiratory infections and skin infections. The addition of clavulanate helps overcome bacterial resistance to amoxicillin.
4. Levofloxacin
Levofloxacin, another fluoroquinolone, is sometimes used as an alternative to ciprofloxacin. It has a broader spectrum of activity and is effective against a variety of pathogens. However, it shares similar side effects and resistance concerns.
Non-Antibiotic Alternatives
In some cases, non-antibiotic treatments may be appropriate, especially for mild infections or when antibiotics are contraindicated. These include:
- Topical antiseptics for skin infections
- Probiotics to restore gut flora after antibiotic use
- Hydration and rest for viral infections
Case Studies and Statistics
A study published in the Journal of Antimicrobial Chemotherapy found that nitrofurantoin was effective in treating uncomplicated UTIs in 90% of cases, with significantly lower resistance rates compared to ciprofloxacin. Another research indicated that the use of TMP-SMX has decreased due to rising resistance, highlighting the importance of susceptibility testing before treatment.
Considerations for Choosing Alternatives
When selecting an alternative to ciprofloxacin, healthcare providers should consider:
- The type of infection and its severity
- Patient history and potential allergies
- Local resistance patterns
- Potential side effects and drug interactions
Conclusion
As antibiotic resistance continues to pose a significant threat to public health, exploring alternatives to ciprofloxacin is crucial. Options such as nitrofurantoin, TMP-SMX, and amoxicillin-clavulanate offer effective treatment for various infections while minimizing the risk of resistance. Additionally, non-antibiotic treatments can be beneficial in certain scenarios. Ultimately, the choice of antibiotic should be guided by clinical judgment, susceptibility testing, and patient-specific factors to ensure optimal outcomes.