-
Table of Contents
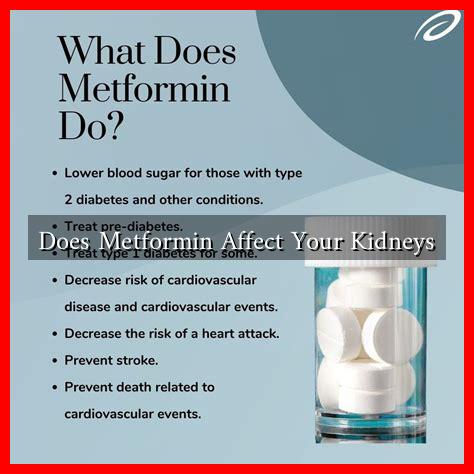
Does Metformin Affect Your Kidneys?
Metformin is a widely prescribed medication for managing type 2 diabetes. It helps lower blood sugar levels and is often the first-line treatment for this condition. However, concerns about its effects on kidney health have emerged over the years. This article delves into the relationship between metformin and kidney function, exploring both the potential risks and benefits.
Understanding Metformin
Metformin works primarily by decreasing glucose production in the liver and improving insulin sensitivity. It is generally well-tolerated, but like any medication, it can have side effects. One of the most significant concerns is its impact on the kidneys, particularly in patients with pre-existing kidney conditions.
How Metformin Affects Kidney Function
Research indicates that metformin is generally safe for the kidneys when used appropriately. However, there are specific scenarios where it can pose risks:
- Renal Impairment: Patients with reduced kidney function may experience an accumulation of metformin, leading to a rare but serious condition known as lactic acidosis.
- Dehydration: Conditions that lead to dehydration, such as severe infections or gastrointestinal issues, can exacerbate kidney problems when taking metformin.
- Contrast-Induced Nephropathy: Patients undergoing imaging procedures that require contrast dye should temporarily discontinue metformin to prevent kidney damage.
Research Findings
Numerous studies have examined the effects of metformin on kidney health. A notable study published in the Journal of Diabetes Research found that metformin does not significantly increase the risk of kidney disease in patients with type 2 diabetes. In fact, it may even have protective effects on kidney function over time.
Another study published in the American Journal of Kidney Diseases indicated that metformin use was associated with a lower risk of developing chronic kidney disease (CKD) compared to other diabetes medications. This suggests that, for many patients, metformin may be a safer option for managing diabetes without compromising kidney health.
Case Studies and Statistics
Several case studies highlight the importance of monitoring kidney function in patients taking metformin:
- A case study involving a 65-year-old woman with type 2 diabetes and stage 3 CKD showed that her kidney function remained stable over two years while on metformin, provided her renal function was regularly monitored.
- Statistics from the Centers for Disease Control and Prevention (CDC) indicate that approximately 30% of adults with diabetes have CKD, underscoring the need for careful management of both conditions.
Guidelines for Safe Use
To minimize the risks associated with metformin and kidney health, healthcare providers recommend the following guidelines:
- Regularly monitor kidney function, especially in older adults or those with pre-existing kidney issues.
- Adjust metformin dosage based on renal function, following the guidelines provided by the American Diabetes Association.
- Educate patients about the signs of lactic acidosis, such as unusual fatigue, muscle pain, and difficulty breathing.
Conclusion
In summary, metformin is a cornerstone in the management of type 2 diabetes and, when used appropriately, poses minimal risk to kidney health. While there are specific circumstances where caution is warranted, the overall evidence suggests that metformin can be safely used in patients with well-monitored kidney function. Regular check-ups and open communication with healthcare providers are essential for ensuring the safe use of this medication. As always, patients should consult their doctors before making any changes to their medication regimen.