-
Table of Contents
Can Diclofenac Worsen Existing Gut Problems?
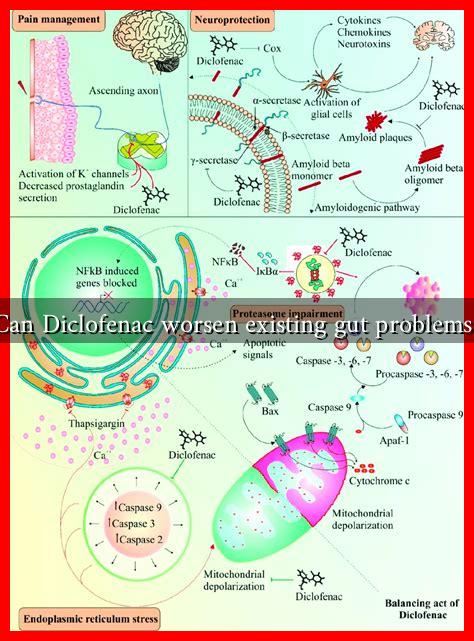
Diclofenac is a non-steroidal anti-inflammatory drug (NSAID) commonly used to relieve pain and reduce inflammation. While it is effective for various conditions, including arthritis and acute pain, concerns have arisen regarding its impact on gastrointestinal health. This article explores whether diclofenac can exacerbate existing gut problems, examining the mechanisms involved, potential risks, and alternative options for pain management.
Understanding Diclofenac and Its Mechanism of Action
Diclofenac works by inhibiting the production of prostaglandins, which are chemicals in the body that promote inflammation, pain, and fever. By blocking the enzyme cyclooxygenase (COX), diclofenac reduces these symptoms effectively. However, prostaglandins also play a crucial role in maintaining the protective lining of the gastrointestinal (GI) tract. When their production is inhibited, the gut may become more susceptible to damage.
The Link Between Diclofenac and Gut Health
Research indicates that NSAIDs, including diclofenac, can lead to various gastrointestinal issues. The following points highlight the potential risks associated with diclofenac use:
- Increased Risk of Ulcers: Studies have shown that long-term use of diclofenac can increase the risk of developing peptic ulcers. A meta-analysis published in the Journal of Gastroenterology found that NSAIDs are responsible for a significant percentage of ulcer-related complications.
- Gastrointestinal Bleeding: Diclofenac can cause gastrointestinal bleeding, particularly in individuals with pre-existing gut issues. A study in the American Journal of Gastroenterology reported that NSAID use is a major risk factor for upper GI bleeding.
- Exacerbation of Inflammatory Bowel Disease (IBD): For patients with conditions like Crohn’s disease or ulcerative colitis, diclofenac may worsen symptoms. A study indicated that NSAIDs could trigger flare-ups in IBD patients, leading to increased abdominal pain and diarrhea.
Case Studies and Statistics
Several case studies illustrate the potential dangers of diclofenac for individuals with existing gut problems. For instance, a 2018 case report detailed a patient with a history of peptic ulcers who experienced severe gastrointestinal bleeding after starting diclofenac therapy. This case underscores the importance of careful monitoring and consideration of alternative treatments for patients with a history of gut issues.
Statistics further emphasize the risks associated with diclofenac. According to the World Health Organization, NSAIDs are responsible for approximately 30% of all hospitalizations due to gastrointestinal complications. This statistic highlights the need for caution when prescribing diclofenac, especially to patients with pre-existing gut conditions.
Alternatives to Diclofenac for Pain Management
Given the potential risks associated with diclofenac, patients with existing gut problems should consider alternative pain management strategies. Some options include:
- Acetaminophen: Often recommended as a safer alternative for pain relief, acetaminophen does not have the same gastrointestinal side effects as NSAIDs.
- Topical NSAIDs: These can provide localized pain relief without significantly affecting the gastrointestinal tract.
- Physical Therapy: Non-pharmacological approaches, such as physical therapy, can help manage pain without the risks associated with medications.
Conclusion
In summary, while diclofenac is an effective pain reliever, it poses significant risks for individuals with existing gut problems. The potential for increased gastrointestinal complications, including ulcers and bleeding, necessitates careful consideration before prescribing this medication. Patients with a history of gut issues should discuss alternative pain management strategies with their healthcare providers to ensure their safety and well-being. Understanding the implications of diclofenac use is crucial for making informed decisions about pain management.