-
Table of Contents
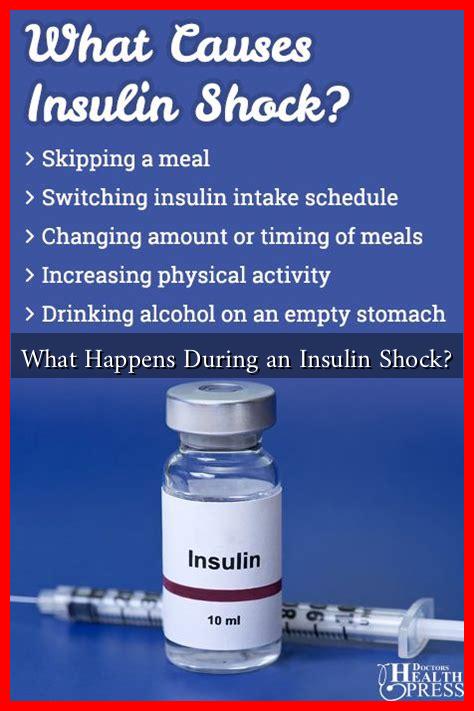
What Happens During an Insulin Shock?
Insulin shock, also known as hypoglycemia, occurs when blood sugar levels drop dangerously low due to an excess of insulin in the body. This condition is particularly relevant for individuals with diabetes who use insulin therapy. Understanding the physiological processes, symptoms, and potential treatments for insulin shock is crucial for managing diabetes effectively and preventing severe complications.
Understanding Insulin and Blood Sugar Regulation
Insulin is a hormone produced by the pancreas that plays a vital role in regulating blood glucose levels. It facilitates the uptake of glucose by cells, providing them with the energy needed for various bodily functions. When insulin levels are too high, or when there is insufficient glucose available, hypoglycemia can occur. This condition can be triggered by several factors, including:
- Excessive insulin administration
- Missed meals or inadequate food intake
- Intense physical activity
- Alcohol consumption
Symptoms of Insulin Shock
The symptoms of insulin shock can vary in severity and may develop rapidly. Early signs often include:
- Shakiness or trembling
- Excessive sweating
- Rapid heartbeat
- Hunger
- Headaches
If left untreated, hypoglycemia can progress to more severe symptoms, such as:
- Confusion or disorientation
- Seizures
- Loss of consciousness
- Coma
According to the American Diabetes Association, hypoglycemia is defined as a blood glucose level below 70 mg/dL. However, individual responses to low blood sugar can vary, and some people may experience symptoms at higher levels.
Case Studies: Real-Life Implications of Insulin Shock
Understanding insulin shock through real-life examples can provide valuable insights into its impact. For instance, a study published in the journal *Diabetes Care* highlighted a case where a 45-year-old man with Type 1 diabetes experienced recurrent hypoglycemic episodes. Despite being educated about the signs and symptoms, he often mismanaged his insulin doses, leading to severe hypoglycemia that required emergency intervention.
Another case involved a young athlete with Type 1 diabetes who experienced insulin shock during a marathon. His failure to consume adequate carbohydrates before the race resulted in a rapid drop in blood sugar levels, leading to confusion and disorientation mid-race. Fortunately, he was assisted by fellow runners who provided him with glucose tablets, averting a more serious crisis.
Treatment and Management of Insulin Shock
Immediate treatment for insulin shock is crucial to prevent severe complications. Here are some common strategies:
- Consume Fast-Acting Carbohydrates: Foods or drinks containing glucose, such as fruit juice, candy, or glucose tablets, can quickly raise blood sugar levels.
- Glucagon Injection: In severe cases where the individual is unconscious or unable to swallow, a glucagon injection can be administered by a bystander or caregiver to raise blood sugar levels.
- Follow-Up Care: After an episode, it is essential to monitor blood sugar levels and consult a healthcare provider to adjust insulin dosages or dietary plans.
Preventing Insulin Shock
Preventing insulin shock involves a combination of education, monitoring, and lifestyle adjustments. Here are some effective strategies:
- Regularly monitor blood glucose levels to identify patterns and prevent lows.
- Maintain a balanced diet that includes carbohydrates, proteins, and fats.
- Educate family and friends about recognizing the signs of hypoglycemia and how to respond.
- Carry a source of fast-acting carbohydrates at all times.
Conclusion
Insulin shock is a serious condition that can have life-threatening consequences if not managed properly. Understanding the symptoms, treatment options, and preventive measures is essential for individuals with diabetes and their caregivers. By staying informed and prepared, those at risk can significantly reduce the likelihood of experiencing hypoglycemia and maintain better overall health. For more information on managing diabetes and preventing hypoglycemia, visit the American Diabetes Association.